1、简介
干扰素(IFN)多效性细胞因子家族,根据受体特异性可分为三型:I型(含IFN-α/β等13个亚型,通过IFNAR1/IFNAR2受体传递信号)、II型(仅包含IFN-γ,特异性结合IFNGR1/IFNGR2受体)及III型(IFN-λ,依赖IL-10R2/IFNLR1受体发挥作用)[1-2]。IFN-γ是Ⅱ型干扰素的唯一成员,其基因定位于人类染色体12q15区域,包含4个外显子,其编码基因在脊椎动物中呈现高度保守性(人鼠氨基酸序列同源性约70%)。编码的成熟蛋白由143个氨基酸通过链间二硫键形成功能性同源二聚体,其受体结合域中保守的α螺旋结构对生物活性至关重要[3]。
IFN-γ主要由T淋巴细胞、自然杀伤细胞(NK)和抗原提呈细胞(APCs,包括单核细胞、巨噬细胞和树突状细胞)分泌[4-6]。其表达受先天免疫信号的严格调控,APCs通过分泌IL-12/IL-18激活STAT4/NF-κB通路,一方面趋化NK细胞向炎症部位迁移,另一方面直接诱导IFN-γ基因转录,形成连接病原识别与适应性免疫启动的关键调控轴[7-9]。
作为免疫微环境的核心调控者,IFN-γ在感染部位呈现爆发式表达特征,其通过激活巨噬细胞杀菌功能、上调MHC分子表达及驱动Th1分化等机制增强宿主防御[10]。同时,该因子在肿瘤免疫中发挥双重作用:既可诱导肿瘤细胞免疫原性死亡,又能促进免疫检查点分子(如PD-L1)表达形成负反馈调控[11]。这种功能复杂性与其独特的信号级联机制直接相关,IFN-γ通过结合异源二聚体受体(IFNGR1/IFNGR2),触发JAK1/JAK2-STAT1磷酸化级联反应,磷酸化STAT1入核后协同IRF家族蛋白,通过结合干扰素刺激反应元件(ISRE)启动数百种干扰素刺激基因(ISGs)转录,形成级联放大效应。
2、功能或作用机制
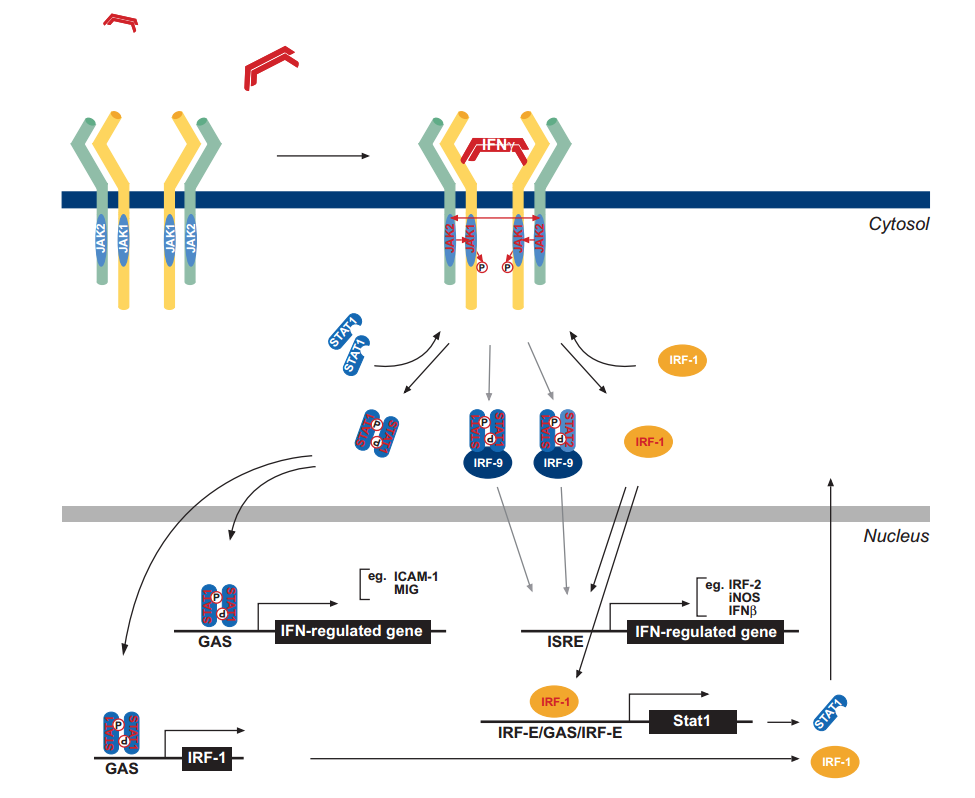
1)受体激活与激酶级联
IFN-γ以同源二聚体形式结合异源二聚体受体IFNGR,诱导受体构象变化。此过程激活受体偶联的JAK1(结合IFNGR2)和JAK2(结合IFNGR1)酪氨酸激酶,触发二者相互磷酸化。活化的JAK1进一步磷酸化IFNGR1链第440位酪氨酸残基(Y440),形成两个相邻的STAT1蛋白SH2结构域结合位点[12-14]。
2)STAT1磷酸化与复合物组装
募集至受体的STAT1分子在其C端Y701位点被JAK激酶磷酸化,激活诱导STAT1同源二聚化并从受体解离,同源二聚体进一步激活激活IRF-1(Interferon Regulatory Factor-1,干扰素调节因子-1)及IFN-γ激活序列(GAS),以启动后续的基因转录调控,而少部分受体解离的STAT1会与STAT2及IRF-9形成异源复合物[15-17]。其中,STAT1:STAT1:IRF-9复合物调控经典GAS(IFN-γ-激活序列)响应基因;STAT1:STAT2:IRF-9(ISGF3复合物):靶向ISRE(干扰素刺激反应元件)
3)核转位与基因转录调控
磷酸化Stat1同源二聚体与ISGF3复合物转位入核,分别结合靶基因启动子区的GAS和ISRE元件[18]。IRF-1作为次级转录因子,进一步扩大调控网络。此过程激活包括ICAM-1(细胞间黏附分子)、iNOS(诱导型一氧化氮合酶)及IRF家族成员在内的多种干扰素调控基因,形成多层级转录放大效应。
3、临床应用
1)抗感染
IFN-γ作为一种重要的免疫调节因子,在抗感染过程中发挥着关键作用。它通过激活巨噬细胞,增强其吞噬和杀伤能力,促进抗原提呈,从而提高机体对病原体的清除效率[20]。此外,IFN-γ还能诱导产生抗菌肽和其他具有直接杀菌作用的分子,进一步加强宿主防御功能。
2)抗肿瘤
IFN-γ在肿瘤免疫监视中占据核心地位,能够直接抑制肿瘤细胞增殖,并通过多种途径增强机体的抗肿瘤免疫反应。IFN-γ可以上调MHC I类分子表达,使肿瘤细胞更容易被识别;刺激NK细胞、T细胞等效应细胞的活性;诱导免疫检查点分子如PD-L1的表达,进而调节肿瘤微环境中的免疫平衡[11,21-22]。
3)自身免疫性疾病
过度活跃的IFN-γ信号可能导致自身免疫性疾病的发生和发展,如系统性红斑狼疮(SLE)、多发性硬化症(MS)等[23-24]。针对IFN-γ信号通路的关键节点进行干预,如使用单克隆抗体阻断IFN-γ与其受体结合,或设计小分子化合物抑制下游信号传导,可有效控制病情进展,减少并发症。
4)移植排斥反应
器官移植术后,供体与受体之间的HLA(Human Leukocyte Antigen,人类白细胞抗原)差异是引发急性排斥反应的主要原因。IFN-γ在此过程中扮演重要角色,它能增强移植物特异性T细胞的活化,加剧局部炎症反应,最终导致移植物功能丧失。IFN-γ抑制药物可下调移植排斥介导的免疫应答。此外,IL-10等具有抗炎效果的细胞因子,可以作为潜在的治疗策略,减轻IFN-γ带来的不利影响[25]。
5)神经退行性疾病
IFN-γ在神经退行性疾病如阿尔茨海默病(AD)、帕金森病(PD)中显示出复杂的双重作用。一方面,适度的IFN-γ水平有助于清除β-淀粉样蛋白沉积物,减缓疾病进程;另一方面,过量的IFN-γ可能会加重神经炎症,损害神经元结构与功能[26]。针对IFN-γ在神经退行性疾病中的复杂角色,未来的研究需要更加细致地解析其调控网络,以期找到既能利用其有益效应又能避免不良后果的治疗方案。
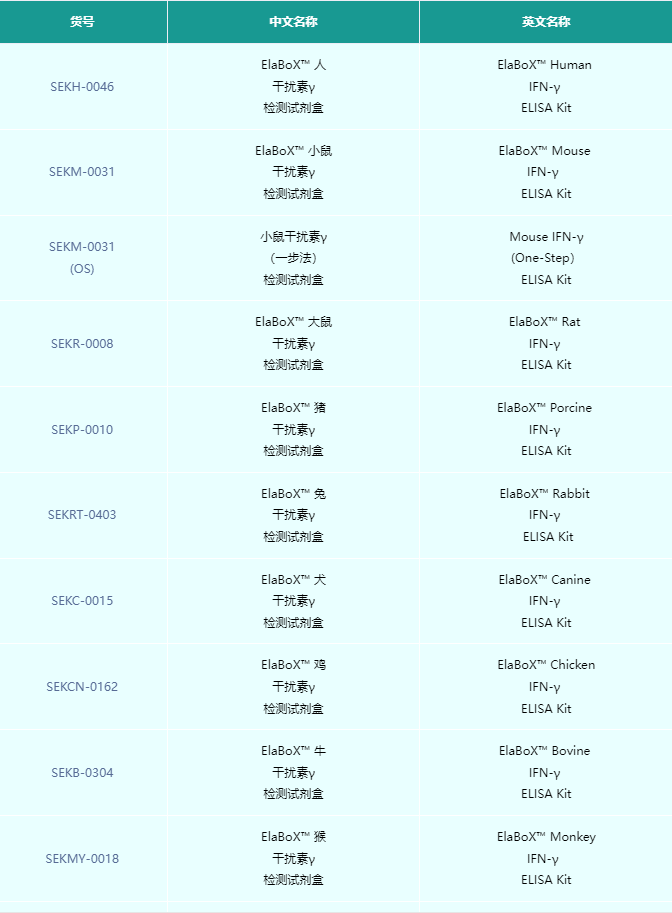
相关产品
参考文献
[1] Bazan, J. F. (1990) Structural design and molecular evolution of a cytokine receptor superfamily. Proc. Natl. Acad. Sci. USA 87, 6934– 6938.
[2] Thoreau, E., Petridou, B., Kelly, P. A., Djiane, J., Mornon, J. P. (1991) Structural symmetry of the extracellular domain of the cytokine/growth hormone/prolactin receptor family and interferon receptors revealed by hydrophobic cluster analysis. FEBS Lett. 282, 26–31.
[3] Adolf, G. R. (1985) Structure and effects of interferon-gamma. Oncology 42, 1–10.
[4] Carnaud, C., Lee, D., Donnars, O., Park, S. H., Beavis, A., Koezuka, Y., Bendelac, A. (1999) Cutting edge: cross-talk between cells of the innate immune system: NKT cells rapidly activate NK cells. J. Immunol. 163, 4647–4650.
[5] Frucht, D. M., Fukao, T., Bogdan, C., Schindler, H., O’Shea, J. J., Koyasu, S. (2001) IFN-gamma production by antigen-presenting cells: mechanisms emerge. Trends Immunol. 22, 556–560.
[6] Gessani, S., Belardelli, F. (1998) IFN-gamma expression in macrophages and its possible biological significance. Cytokine Growth Factor Rev. 9,117–123.
[7] Munder, M., Mallo, M., Eichmann, K., Modolell, M. (1998) Murine
macrophages secrete interferon gamma upon combined stimulation with
interleukin (IL)-12 and IL-18: a novel pathway of autocrine macrophage
activation. J. Exp. Med. 187, 2103–2108.
[8] Fukao, T., Matsuda, S., Koyasu, S. (2000) Synergistic effects of IL-4 and IL-18 on IL-12-dependent IFN-gamma production by dendritic cells.
J. Immunol. 164, 64–71.
[9] Schindler, H., Lutz, M. B., Rollinghoff, M., Bogdan, C. (2001) The
production of IFN-gamma by IL-12/IL-18-activated macrophages requires STAT4 signaling and is inhibited by IL-4. J. Immunol. 166,
3075–3082.
[10] Bach, E. A., Szabo, S. J., Dighe, A. S., Ashkenazi, A., Aguet, M., Murphy,K. M., Schreiber, R. D. (1995) Ligand-induced autoregulation of IFNgamma receptor beta chain expression in T helper cell subsets. Science 270, 1215–1218.
[11] Kaplan, D. H., Shankaran, V., Dighe, A. S., Stockert, E., Aguet, M., Old, L. J., Schreiber, R. D. (1998) Demonstration of an interferon gamma dependent tumor surveillance system in immunocompetent mice. Proc. Natl. Acad. Sci. USA 95, 7556–7561.
[12] Greenlund, A.C., Farrar, M.A., Viviano, B.L., Schreiber, R. D. (1994) Ligand-induced IFN gamma receptor tyrosine phosphorylation couples the receptor to its signal transduction system (p91). EMBO J. 13, 1591–1600.
[13] Briscoe, J., Rogers, N. C., Witthuhn, B. A., Watling, D., Harpur, A.G., Wilks, A.F., Stark, G.R. , Ihle , J.N. ,Kerr,I.M. (1996) Kinase-negative mutants of JAK1 can sustain interferon-gamma-inducible gene expression but not an antiviral state. EMBO J. 15, 799–809.
[14] Igarashi, K., Garotta, G., Ozmen, L., Ziemiecki, A., Wilks, A. F., Harpur, A. G., Larner, A. C., Finbloom, D. S. (1994) Interferon-gamma induces tyrosine phosphorylation of interferon-gamma receptor and regulated association of protein tyrosine kinases, Jak1 and Jak2, with its receptor. J. Biol. Chem. 269, 14333–14336.
[15] Darnell Jr., J. E., Kerr, I. M., Stark, G. R. (1994) Jak-STAT pathways and transcriptional activation in response to IFNs and other extracellular signaling proteins. Science 264, 1415–1421.
[16] Schindler, C., Darnell Jr., J. E. (1995) Transcriptional responses to polypeptide ligands: the JAK-STAT pathway. Annu. Rev. Biochem. 64,
621–651.
[17] Ramana, C.V., Chatterjee-Kishore, M., Nguyen, H., Stark, G. R. (2000) Complex roles of Stat1 in regulating gene expression. Oncogene 19, 2619–2627
[18] Paludan, S.R. (1998)Interleukin-4 and interferon-gamma: the quintessence of a mutual antagonistic relationship. Scand. J. Immunol. 48,459–468.
[19] Schroder, K., Hertzog, P. J., Ravasi, T., and Hume, D. A. (2003) Interferon-γ: an overview of signals, mechanisms and functions. J. Leukoc. Biol. 75, 163–189. doi:10.1189/jlb.0603252
[20] Davies, E. G., Isaacs, D., Levinsky, R. J. (1982) Defective immune interferon production and natural killer activity associated with poor neutrophil mobility and delayed umbilical cord separation. Clin. Exp. Immunol. 50, 454–460.
[21] Dighe, A. S., Richards, E., Old, L. J., Schreiber, R. D. (1994) Enhanced in vivo growth and resistance to rejection of tumor cells expressing dominant negative IFN gamma receptors. Immunity 1, 447–456.
[22] Tannenbaum, C. S., Hamilton, T. A. (2000) Immune-inflammatory mechanisms in IFNgamma-mediated anti-tumor activity. Semin. Cancer Biol. 10, 113–123.
[23] Lee, J. Y., Goldman, D., Piliero, L. M., Petri, M., Sullivan, K. E. (2001)Interferon-gamma polymorphisms in systemic lupus erythematosus. Genes Immun. 2, 254–257.
[24] Baechler, E. C., Batliwalla, F. M., Karypis, G., Gaffney, P. M., Ortmann, W. A., Espe, K. J., Shark, K. B., Grande, W. J., Hughes, K. M., Kapur, V., Gregersen, P. K., Behrens, T. W. (2003) Interferon-inducible gene expression signature in peripheral blood cells of patients with severe lupus. Proc. Natl. Acad. Sci. USA 100, 2610–2615.
[25] Soyoz, M., Pehlivan, M., Tatar, E., Cerci, B., Coven, H. I. K., and Ayna, T. K. (2021) Consideration of IL-2, IFN-γ and IL-4 expression and methylation levels in CD4+ T cells as a predictor of rejection in kidney transplant. Transpl. Immunol. 68, 101414. doi:10.1016/j.trim.2021.101414
[26] Baik, S. H., Kang, S., Lee, W., Choi, H., Chung, S., Kim, J.-I., and Mook-Jung, I. (2019) A Breakdown in Metabolic Reprogramming Causes Microglia Dysfunction in Alzheimer's Disease. Cell Metab. 30(3), 493–507. doi:10.1016/j.cmet.2019.06.005
